5 Essential Tips to Soothe and Manage Eczema-Prone Skin in Lahore
Living with eczema-prone skin can be challenging – especially in a city like Lahore where the climate swings from scorching summers to dry, chilly winters. If you’re in Lahore, you know the hot temperatures and humid monsoon can make you sweat, while the dry, polluted winter air can leave your skin parched and irritated. These conditions can aggravate eczema, leading to itchy, inflamed flare-ups that disrupt your daily life. The good news is that with the right skincare habits and lifestyle tweaks, you can soothe your skin and keep eczema under control. In this guide, we’ll walk through 5 essential tips for managing eczema-prone skin in Lahore, all in a friendly, conversational tone.
From daily moisturizing to avoiding triggers like harsh weather and soaps, we’ve got you covered with practical advice. Let’s dive in and help you find relief, so you can feel comfortable in your own skin year-round.
Table of Contents
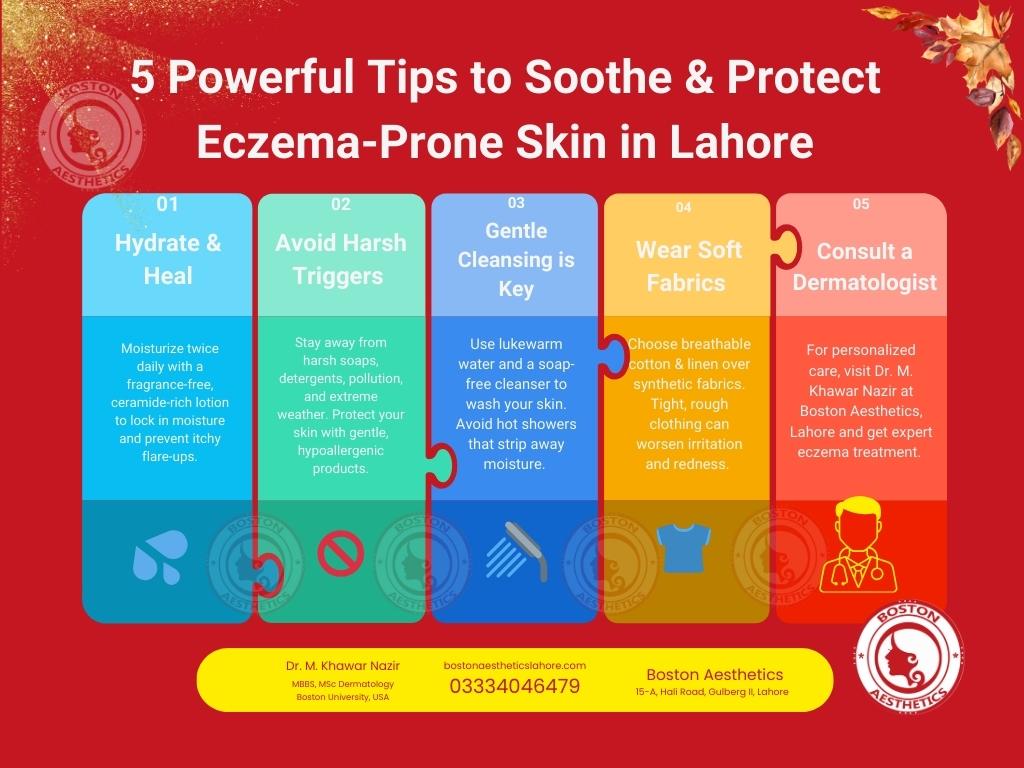
Summary: 5 Essential Tips for Managing Eczema-Prone Skin in Lahore
Suffering from eczema-prone skin? You’re not alone! The itching, redness, and irritation can make daily life uncomfortable, but with the right skincare routine, you can take control and protect your skin. Here are 5 expert-backed tips to help you soothe, heal, and prevent eczema flare-ups in Lahore’s challenging climate.
1️⃣ Keep Your Skin Hydrated – Moisturize Like a Pro!
🔹 Dry, irritated skin? Hydration is the key to relief! Apply a fragrance-free moisturizer with ceramides or shea butter twice a day, especially after bathing, to lock in moisture and prevent itching.
2️⃣ Identify & Avoid Triggers – Say Goodbye to Flare-Ups!
🔹 Weather, pollution, harsh soaps, or stress—these silent triggers can worsen eczema. Switch to gentle, hypoallergenic skincare products, wear a mask on smoggy days, and practice stress management for flare-free skin!
3️⃣ Gentle Cleansing Routine – No More Harsh Soaps!
🔹 Ditch hot showers and strong cleansers—they strip away moisture and worsen eczema! Use lukewarm water and a mild, soap-free cleanser to gently cleanse your skin without irritation.
4️⃣ Wear Soft, Breathable Clothing – Comfort Your Skin!
🔹 Synthetic fabrics = more itching! Choose cotton or linen for everyday wear. Avoid tight clothes, rough fabrics, and scratchy seams that can trigger irritation and inflammation.
5️⃣ Consult a Skin Specialist – Get Expert Care in Lahore!
🔹 When home remedies aren’t enough, professional help makes all the difference! Book an appointment with Dr. M. Khawar Nazir, an American-trained dermatologist at Boston Aesthetics, Lahore, for personalized eczema treatment and long-term relief.
💡 Take Action Today!
Eczema doesn’t have to control your life. Follow these 5 essential tips for managing eczema-prone skin in Lahore, and take the first step towards softer, healthier, and irritation-free skin!
📍 Need expert advice? Book your consultation today at Boston Aesthetics, Lahore, and let Dr. M. Khawar Nazir help you achieve long-term eczema relief. Your skin deserves the best! 💙
1. Moisturize Regularly
One of the golden rules for caring for eczema-prone skin is to moisturize, moisturize, moisturize! Keeping your skin well-hydrated is crucial in preventing dryness and itchiness. Dermatologists often emphasize that moisturizing is a foundational step in eczema treatment for all severities because it helps repair the skin’s protective barrier.
In Lahore’s dry winter or in air-conditioned environments, skin can lose moisture quickly. Applying a good moisturizer regularly ensures your skin stays supple and less prone to cracks or flare-ups.
Choose the right moisturizer: Opt for thick, bland emollients like creams or ointments rather than light lotions. Products that are fragrance-free and hypoallergenic are best, since perfumes and harsh chemicals can irritate sensitive skin. Look for ingredients that lock in moisture – ceramides, glycerin, or shea butter are great for eczema-prone skin. Plain petroleum jelly (Vaseline) is also an excellent occlusive moisturizer that traps water in the skin. In the summer, if heavy ointments feel too greasy, you can use a lighter cream but still make sure it’s alcohol-free and fragrance-free.
Make it a daily habit: Aim to moisturize at least twice a day – for example, once in the morning and once at night. Always moisturize immediately after bathing or washing your hands. Pat your skin lightly with a towel (leave it a bit damp) and then apply your moisturizer within 3 minutes to “lock in” the water before it evaporates. This technique is often referred to as the “soak and seal” method.
Consistency is key: even on days when your eczema isn’t flaring, keep up with moisturizing to strengthen your skin barrier.
Hydrate from the inside and outside: Don’t forget to drink plenty of water throughout the day – staying hydrated can support your skin’s moisture from the inside. In Lahore’s hot climate, you might sweat and lose fluids, so keep a water bottle handy. If the indoor air is very dry (for instance, during winter or in heated rooms), using a humidifier at home can add moisture to the air and prevent your skin from drying out. Every little step helps. By maintaining a regular moisturizing routine, you’ll notice your skin feels softer, less itchy, and better protected against eczema flare-ups.

2. Identify and Avoid Triggers
Eczema often acts up when it’s triggered by something in your environment or daily routine. Part of managing eczema-prone skin is playing detective and learning what makes your skin flare so you can avoid or minimize those triggers. Everyone’s triggers can be a bit different, but there are some common culprits to watch for.
Watch the weather: Lahore’s climate itself can be a trigger. In the dry, cold winter, the low humidity and dusty smoggy air can sap moisture from your skin, leading to irritation.
On the flip side, the intense heat of summer (and the accompanying sweat) can also provoke eczema rashes – sweat and overheating often lead to the dreaded itch. To cope, adapt your routine to the season. In winter, run a humidifier if possible and apply extra-rich moisturizer to combat dryness. In summer, try to stay cool: use fans or air-conditioning, wear breathable clothing, and rinse off sweat promptly (followed by moisturizer) so it doesn’t sit on your skin.
During heavy pollution or smog days (common in Lahore’s winter), limit your outdoor exposure if you notice the polluted air makes you itchy or causes redness. Indoor air purifiers or even just keeping windows closed during peak smog hours can protect your skin from irritants in the air.
Common irritants and allergens: Many everyday products and substances can trigger eczema. Harsh soaps, detergents, and cleaning chemicals are big ones – they strip away the natural oils from your skin. Switch to mild, fragrance-free cleansers and detergents labeled for sensitive skin. Avoid fabric softeners or strong household cleaners with bleach or ammonia, as their residue can irritate your skin. Dust mites and pollen are common allergens that can worsen eczema for some people.
Keep your living space clean: regular dusting, vacuuming, and washing of bed linens in hot water can reduce dust mites. If pollen or outdoor allergens bother you (for example, during spring blooms), rinse off and change clothes after coming in from outside to avoid carrying pollen on your skin. Pet dander (from cats or dogs) is another trigger for some – if you have pets, vacuum often and wash your hands after petting them.
Lahore’s urban environment often means exposure to dust, smoke, and smog, which can trigger eczema flare-ups. Protect your skin from air pollution by wearing a mask outdoors on high-smog days and using air purifiers indoors if possible.

Stress and lifestyle factors: Believe it or not, stress can be a trigger for eczema flare-ups in many people. When you’re anxious or not sleeping well, your skin might respond with more itching and redness. Try to manage stress through relaxation techniques that work for you – whether it’s prayer, yoga, deep breathing, or a hobby you enjoy.
Getting enough sleep is also important; eczema can worsen if your body is run-down. Additionally, be mindful of sweat as a trigger: exercising is great for health, but try to do it in a cool environment and wear moisture-wicking clothes, and shower soon after to remove sweat from your skin.
Keep a little “eczema diary” if you can. Note what you ate, your activities, weather, and products used each day along with how your skin felt. Over time, you might spot patterns (for example, “Whenever I eat spicy foods and then get sweaty, I itch more,” or “My skin is worse after I wear my wool sweater”). Identifying triggers empowers you to avoid or mitigate them.
While you can’t control everything (you can’t change the weather, unfortunately!), small adjustments – like using gentle products, keeping cool, and steering clear of known irritants – will go a long way in preventing those unwelcome eczema flares.
3. Gentle Cleansing Routine
How you cleanse your skin can make a big difference in managing eczema. People with eczema-prone skin have a weaker skin barrier, so harsh cleansing can strip away the natural oils and leave skin even more vulnerable. The goal is to get clean without aggravating your eczema. That means being gentle and thoughtful every time you bathe or wash.
Use lukewarm water, not hot: After a long day, a steaming hot shower might sound tempting – but for eczema, hot water is a no-go. Hot water can dry out your skin and increase inflammation. Stick to lukewarm water for showers and baths. It’s more skin-friendly and will cleanse you without stripping as much moisture. Keep your bath or shower short (around 5–10 minutes is enough to get clean without over-soaking). Remember, bathing actually hydrates the skin with water, but if you stay too long, it can have the opposite effect and dry you out once you step out.
Choose a mild cleanser: Skip the perfumed soaps and deodorant body washes that lather into heaps of foam – those often contain detergents (like SLS) and alcohols that can irritate and dry the skin. Instead, pick a gentle, soap-free cleanser or a hypoallergenic bath oil. Look for words like “gentle cleanser,” “fragrance-free,” “for sensitive skin,” or “pH-balanced” on the product label.
Baby cleansers or washes for sensitive skin can work well for adults with eczema too (no shame in borrowing the baby soap!). You don’t need to soap your entire body head to toe; just focus on the essential areas (armpits, groin, feet, etc.) and where you might have dirt or sweat. Areas that are unaffected by eczema can often be cleansed with just water or very minimal cleanser. During severe flares, some dermatologists even suggest washing less frequently or only with water on the affected areas to avoid irritation.

Gentle technique: When washing, avoid scrubbing your skin aggressively. That means no rough washcloths, loofahs, or exfoliating scrubs on eczema patches. Use your hands or a very soft cloth to gently cleanse. Rubbing or scrubbing can trigger itching and damage the skin barrier. Also, be cautious with your shampoo and facial cleansers – as the runoff can hit your body; choose gentle versions of those too if your eczema extends to the neck or shoulders.
After you’re done, pat your skin dry with a soft towel instead of brisk rubbing.
Leave the skin a bit damp. This is the perfect time to immediately apply your moisturizer (remember the 3-minute rule from Tip #1). This locks in all the water your skin just absorbed. Think of it like “sealing” your skin to prevent evaporation. If you have any prescribed topical medication (like a cream for eczema), apply it to affected areas as directed by your doctor, before you put on your moisturizer. Then slather moisturizer over top and on the rest of your body.
Bonus bath tips: Some people with eczema find colloidal oatmeal baths very soothing (oatmeal can relieve itching). You can buy packets of colloidal oatmeal (or even grind plain oats into a fine powder at home) and add it to your lukewarm bath – it’ll make the water a bit milky and silky feeling, which can calm angry skin.
Just be careful as it can make the tub slippery! Another tip is to avoid bubble baths or strong bath soaps, as fun as bubbles are, because they usually contain fragrances and detergents that can trigger eczema. If you miss the scent, consider adding a few drops of a skin-safe oil (like coconut or sunflower oil) to the bath for a moisturizing effect; but again, no perfumes.
By adopting a gentle cleansing routine, you’ll help your skin stay clean without compromising its natural oils. Many people find that once they switch to lukewarm showers and mild cleansers, their skin feels less tight and itchy after bathing. It’s a simple change with big benefits for eczema management.
- Patient Awareness Campaigns on Steroid-Induced Dermatitis | Boston Aesthetics Lahore
- 5 Proven Ways to Calm Mind & Glow Skin in Lahore
- 5 Steps to Confident Nose Reshaping in Lahore
- 5 Shocking Truths About Lip Laser Rejuvenation
- Does Sunblock Give Complete Sun Protection?
4. Wear Appropriate Clothing
Did you know the clothes you wear can affect your eczema? It’s true – your wardrobe choices can either soothe your skin or secretly irritate it. In Lahore, where temperatures vary greatly, picking the right fabrics and clothing styles is extra important to keep your eczema-prone skin comfortable.
Soft, breathable fabrics are your friends: As a rule of thumb, stick to natural, breathable materials next to your skin. Cotton is a top choice for many people with eczema.
It’s soft, allows your skin to “breathe,” and absorbs sweat, helping you stay cool. In the summer heat, light cotton shirts and loose trousers or shalwar kameez made of cotton can prevent overheating and sweat build-up (which can trigger itching). In winter, cotton can be layered to keep you warm without irritation.
Other eczema-friendly fabrics include linen (great for hot weather) and bamboo-based fabrics – these are also soft and temperature-regulating. Some folks also like silk or silk blends; silk is smooth and can help regulate body temperature, though pure silk can be pricey and a bit hard to care for. There are even special silk and finely-woven garments sold for eczema that reduce friction on the skin.
Avoid irritant materials: On the flip side, wool and synthetic fabrics (like polyester, nylon, acrylic) often spell trouble for eczema.
Wool is a common trigger – those wool fibers can be very scratchy on the skin and cause overheating and sweating which leads to the “itch-scratch cycle.” If you love woolen sweaters in winter, consider wearing a soft cotton layer underneath so the wool never directly touches your skin. Synthetic fabrics (polyester and such) don’t absorb sweat well and can cause heat to get trapped, often leading to itching. They can also have rough fibers or chemicals that irritate the skin.
Try to choose clothing labeled 100% cotton (or a very high percentage of it). Sometimes “cotton-rich” blends still contain a lot of polyester, so check the tag. Also, avoid clothing with rough seams, tags, or tight elastics that constantly rub on your skin. That constant friction can trigger eczema in those areas (for example, a tight waistband or a scratchy tag at the neck). You can cut tags off or wear clothes inside-out at home if seams bother you.

Certain fabrics can irritate eczema-prone skin. The image above shows a man scratching his arm – a familiar scene for anyone whose shirt fabric makes them itchy. Opt for loose, breathable cotton clothes to minimize irritation.
Dress for the weather: In Lahore’s summer, choose lightweight, loose-fitting outfits. Flowy cotton or lawn suits, breathable kurtas, or linen shirts can keep your body cool. Light colors also absorb less heat. If you exercise, look for “moisture-wicking” activewear (these are usually special synthetics that are designed to pull sweat away and feel smooth – some eczema sufferers tolerate these for workouts, but cotton works too).
In winter, layering is key. Instead of one heavy sweater, wear a soft base layer (cotton undershirt or thermal) plus a warmer layer on top. This way if you start overheating, you can remove a layer. Overheating can quickly lead to itchy skin, so it’s better to be slightly cool than too warm. Also, consider scarves, masks or gloves made of cotton if you need to protect your face and hands from cold dry air or dust – just make sure they’re clean and soft.
Laundry matters: It’s not just what you wear, but how you care for it. Wash new clothes before wearing them to remove any excess dyes or factory chemicals. Use a mild, fragrance-free detergent for washing your clothes and bedding (strong detergents can leave residue that irritates skin). You might also add an extra rinse cycle to make sure all detergent is out. Avoid fabric softeners or dryer sheets with fragrance – if you need a softener, there are unscented or sensitive-skin ones available, or you can use white vinegar in the rinse cycle as a natural softener (don’t worry, the vinegar smell goes away).
By wearing comfortable, eczema-friendly clothing, you create a protective layer for your skin. You’ll likely notice less random itching during the day when your clothes aren’t provoking your eczema. Plus, who doesn’t love an excuse to wear soft, cozy fabrics all the time? Your fashion can be both chic and gentle on your skin.
5. Consult a Dermatologist
While careful skincare and avoidance of triggers go a long way, sometimes you need professional guidance for stubborn eczema. Don’t hesitate to consult a dermatologist – especially one experienced with eczema – when your skin is flaring or not improving with home care. A dermatologist (skin specialist) can provide expert advice, identify specific triggers, and prescribe treatments that are safe and effective for eczema-prone skin.
Why see a dermatologist? Eczema can be a complex condition. What works for one person might not work for another. A dermatologist will assess your specific situation – the type of eczema you have, the areas affected, and the severity. They can help you pinpoint triggers (for example, through allergy testing if they suspect you have contact allergies or atopic dermatitis triggers).
They’ll also make sure your skin condition is indeed eczema and not something else. Sometimes infections can occur on eczema-damaged skin, and those might need medical treatment to clear up. A skin doctor can recognize signs of infection (like if your eczema has yellow crusts or is especially painful) and treat it promptly.
In terms of treatment, dermatologists have a toolkit of options. They might recommend or prescribe medicated creams or ointments to calm inflammation (such as low-strength steroid creams or non-steroid anti-inflammatory ointments) – used correctly, these can greatly reduce a severe flare. They can guide you on how to use them safely (for example, how long to apply a steroid cream and on which areas). Importantly, a dermatologist will tailor the treatment to you.
If your eczema is very mild, they might suggest over-the-counter hydrocortisone sparingly and focus more on moisturizers. If it’s more severe, they could discuss advanced options like phototherapy (light therapy) or newer treatments, all while ensuring you understand the benefits and risks. Having professional supervision means you’re using the right treatments at the right time, which can prevent eczema from worsening.
Dr. M. Khawar Nazir at Boston Aesthetics – Lahore’s eczema expert: When seeking a dermatologist in Lahore, you’ll want someone knowledgeable and trustworthy. Dr. M. Khawar Nazir is a highly experienced skin specialist at Boston Aesthetics in Lahore. He is an American-trained dermatologist (with credentials from Boston University, USA) and has years of experience dealing with a wide range of skin conditions, including eczema.
Under his care at Boston Aesthetics, patients receive personalized treatment plans designed for their unique skin needs. Dr. Khawar Nazir understands how Lahore’s environment can affect skin and can provide targeted advice – from recommending the right moisturizers to prescribing appropriate medicated creams when needed. Many patients commend his compassionate, attentive approach and how clearly he explains each step of the care process. With professional guidance, you might discover solutions you hadn’t tried before, or finally get relief after months (or years) of ongoing flare-ups.
Don’t wait for a crisis: It’s wise to consult a dermatologist before your eczema becomes extremely severe. If you notice your usual routine isn’t helping, or the rashes are spreading, blistering, or keeping you up at night with itching, make that appointment. Also, if eczema is affecting your self-esteem or mental health (constant discomfort can be really tough), a dermatologist can help you get it under better control, which can greatly improve your quality of life. Sometimes even a one-time consultation can set you on the right track, giving you a solid game plan for managing your eczema.
Remember, seeking professional help is not a sign of defeat – it’s using every tool available to take care of your health. Alongside your at-home care (the moisturizing, trigger avoidance, gentle cleansing, etc.), expert medical advice can be the missing piece to break the cycle of flares. You deserve relief and healthy skin, and a good dermatologist will be your partner in reaching that goal.
FAQs (Frequently Asked Questions)
Below are answers to some common questions people have about managing eczema-prone skin, especially focusing on lifestyle and skincare tips:
Q1: What triggers eczema flare-ups?
A: Eczema flare-ups can be triggered by a variety of factors. Common triggers include dry weather or low humidity, which can parch your skin, and extreme heat, which causes sweating that leads to itching. Irritants like harsh soaps, detergents, or perfumes are frequent culprits – they can inflame sensitive skin. Allergens such as dust mites, pet dander, pollen, or mold may also provoke eczema in people who are allergic to them.
Additionally, stress and lack of sleep can worsen eczema for some individuals. It’s important to observe your own pattern; keeping a diary of activities, foods, and exposures when you have a flare-up can help identify your personal triggers. Once you know them, you can take steps to avoid or minimize those triggers (for example, using a humidifier in dry weather or switching to fragrance-free household products).
Q2: How often should I moisturize eczema-prone skin?
A: Moisturize at least twice a day – more if your skin feels particularly dry or after any activity that dries you out (like washing your hands or taking a shower). A good routine is to apply a thick moisturizer every morning after you wake up and every night before bed. Also, always moisturize immediately after bathing or washing; pat your skin damp-dry and apply your moisturizer within a few minutes to lock in hydration.
If you’re in an air-conditioned office or heated room for long hours, consider keeping a travel-size moisturizer handy to reapply to itchy or tight areas (like hands, elbows) during the day. Consistent moisturization is one of the most effective ways to manage eczema-prone skin and can significantly reduce flare-ups.
Q3: Are daily baths or showers good or bad for eczema?
A: Daily baths or showers can actually be helpful for eczema-prone skin if done correctly. Bathing hydrates the skin and removes irritants like sweat and allergens, which is good for eczema. The key is to keep the bath/shower short (about 5-10 minutes) and use lukewarm water, not hot. Use a gentle, eczema-friendly cleanser and avoid scrubbing your skin. Right after bathing, apply your moisturizer generously (the “soak and seal” method).
This routine of daily bathing followed by immediate moisturizing helps trap water in the skin and can prevent dryness. However, bathing too long or in hot water or using harsh soaps can dry out the skin and make eczema worse, so those should be avoided. If your eczema is very severe or you have open sores, your dermatologist might give specific bathing instructions. In general, a short, gentle daily bath or shower followed by moisturization is beneficial for most people with eczema.
Q4: What type of soap or cleanser is best for eczema-prone skin?
A: The best cleanser for eczema-prone skin is one that is mild, fragrance-free, and soap-free. Look for cleansers labeled “for sensitive skin” or “gentle hydrating cleanser.” These are usually free of sulfates and harsh detergents that strip your skin’s oils. Avoid traditional bar soaps (they often have a high pH and can be drying) and anything with strong fragrances or antibacterial chemicals. Instead, consider products like gentle skin cleansers, lipid-replenishing washes, or bath oils recommended for eczema.
You don’t need a lot of lather; in fact, less lather usually means less harshness. Brands that make gentle, non-soap cleansers (often recommended by dermatologists) include Cetaphil, CeraVe, Eucerin, and Aveeno – but make sure to choose their fragrance-free products (they often have a specific line for eczema or sensitive skin). Baby washes can also be a good choice since they’re formulated to be gentle. Always rinse off well with lukewarm water, and follow up with moisturizer. Remember, the goal is to cleanse the skin without over-drying it.
Q5: Can my diet affect my eczema?
A: Diet does not cause eczema, but in some people certain foods can trigger or worsen a flare-up due to food sensitivities or allergies. Common food triggers (especially in children with eczema) can include eggs, dairy, wheat, soy, nuts, and seafood, but it’s very individual. If you notice a pattern, such as your eczema itching more after eating a particular food, you might want to discuss with a doctor and possibly get tested for food allergies. That said, not everyone with eczema has food triggers. For many adults, diet might not play a significant role at all. Nonetheless, eating a healthy diet can improve your overall skin health and support your immune system.
Focus on foods rich in Omega-3 fatty acids (like fish, flaxseeds, walnuts) which are anti-inflammatory, and plenty of fruits and vegetables for vitamins. Staying well-hydrated by drinking water is also beneficial for your skin. It might help to keep a food diary if you suspect a link between what you eat and your skin’s behavior. If a certain food consistently seems to flare your eczema, you can try eliminating it (under guidance of a doctor, especially to ensure you maintain proper nutrition). Remember that extreme or “fad” diets are usually not necessary for eczema – a balanced, nutritious diet and identifying any personal food triggers is the way to go.
Q6: Does stress really make eczema worse?
A: Yes, stress can be a trigger for eczema flare-ups in many people. When you’re stressed or anxious, your body releases hormones (like cortisol) that can increase inflammation and itching in the skin. You might have noticed that during exams, work pressures, or emotional ups and downs, your eczema acts up – that’s a common experience. Conversely, having a bad eczema flare can cause stress, creating a bit of a vicious cycle. Managing stress is an important but often overlooked part of eczema care.
Try to incorporate stress-reduction techniques into your routine: this could be deep breathing exercises, meditation, yoga, or even simple practices like taking a walk in a park or listening to calming music. Ensure you’re getting enough sleep, as lack of sleep can stress the body and also give you more urge to scratch. Some people find that talking to a counselor or joining an eczema support group helps them cope better with the emotional toll of chronic itching and discomfort. While eliminating stress completely isn’t realistic (life happens!), finding healthy outlets and relaxation methods can definitely help reduce stress-related flare-ups and improve your overall well-being.
Q7: What fabrics are best (and worst) for eczema-prone skin?
A: Best fabrics: Soft, natural, breathable fabrics are best. 100% cotton is often the top recommendation.
It’s gentle, allows airflow, and absorbs moisture (sweat) from your skin. Linen is another breathable fabric good for hot weather. Bamboo fabric (often labeled as bamboo viscose) is praised for being soft and temperature-regulating – it can keep you cool in summer and warm in winter. Some people also do well with silk, which is very smooth (there are even special therapeutic silk garments for eczema). Tencel (lyocell) is a newer eco-friendly fabric made from wood pulp that’s also quite gentle on the skin. Always wash new clothes before wearing to remove any chemicals and use gentle, fragrance-free laundry detergent.
Worst fabrics: Wool is notoriously bad for eczema – it’s scratchy and can cause overheating and sweating, which triggers itching.
Even fine merino wool can bother some eczema sufferers. If you must wear wool (like a school uniform or sweater), wear a cotton layer underneath. Synthetic fabrics like polyester, nylon, acrylic, and spandex can also irritate because they don’t breathe well and may cause you to sweat or overheat. They also often have chemical dyes or finishes that can be irritating. Rough textures or fabrics with glittery threads, sequins, or tags can rub and irritate the skin as well. In general, go for clothes that feel soft on your skin and aren’t too tight. Loose, breathable clothing made of the “good” fabrics will help reduce friction and let your skin breathe, which means happier skin.
Q8: How can I stop the itching without scratching?
A: Resisting the urge to scratch is so hard – we get it! But scratching can make eczema worse and even cause skin infections, so finding alternatives is important. Here are some tips to stop itching without scratching:
- Moisturize or cool the itch: Frequently, itchiness is a sign your skin is dry or irritated. Applying a cold moisturizer or lotion can soothe the itch. You can even store your moisturizer in the fridge for a cool relief. Alternatively, apply a cool compress or an ice pack (wrapped in a cloth) to the itchy area for a few minutes – the cold sensation distracts from the itch and reduces inflammation.
- Gently pat or tap the skin: Instead of clawing at your skin with nails, use the palm of your hand to gently pat the itchy area. This can give some relief without damage. Some people lightly pinch or press around the itchy spot instead of scratching directly. It’s not as satisfying as a scratch, but it’s safer for the skin.
- Keep your nails short and smooth: Despite your best efforts, you might still scratch in your sleep or without thinking. By keeping your fingernails trimmed short and filed, you’ll do less harm if you do scratch. Some eczema sufferers even wear soft cotton gloves at night to prevent nighttime scratching damage.
- Use anti-itch treatments: There are over-the-counter anti-itch creams (like those with 1% hydrocortisone or calamine lotion) that can help calm the itch. Colloidal oatmeal creams or baths can relieve itching as well. Natural oils like cold-pressed coconut oil can soothe mild itch and also add moisture. For some, an oral antihistamine (like cetirizine or diphenhydramine) at night can reduce itching and help with sleep – but check with a doctor before using those regularly. If your itch is severe, talk to your doctor; there are stronger medications or therapies they can recommend.
- Distract yourself: Engage in an activity that takes your mind off the itch – read a book, play a game, squeeze a stress ball, or do some stretches. Sometimes itchiness gets worse the more we focus on it. Stress or boredom can make you more aware of itching, so staying occupied and calm can help. Techniques like meditation or deep breathing can also reduce the sensation of itch.
Finally, remember that managing your eczema overall (with the tips in this guide) will, over time, reduce the baseline itchiness. When you do feel an itch wave coming on, arm yourself with the above strategies. It’s tough, but each time you resist scratching, you’re doing your skin a huge favor.
Q9: Is eczema contagious?
A: No – eczema is NOT contagious. You cannot “catch” eczema from someone, nor can you give it to anyone through touch. Eczema (atopic dermatitis) is an inflammatory skin condition often linked to genetics and immune responses, not an infection. So if you see someone with eczema rashes, don’t worry about getting it – it’s safe to touch or share hugs. And if you have eczema, you can reassure your friends and family that it’s not something they can catch from you. Sometimes eczema can look angry and red, or even have open sores during bad flares, which might make people wonder if it’s infectious – but it’s not. However, because eczema skin can crack and open, it can get infected by bacteria or viruses (like Staph bacteria or the herpes virus).
If an infection occurs, that specific infection could be contagious (for example, impetigo caused by Staph can spread, or eczema herpeticum caused by herpes virus can spread). But the underlying eczema itself remains non-contagious. Using good hygiene (like not scratching with dirty hands, and covering severe open rashes) is mainly to protect yourself from germs, not others from eczema. So, feel comfortable in social situations – eczema might be frustrating, but it’s nobody’s “fault” and not spread by contact.
Q10: Can eczema be cured or only managed?
A: Currently, there is no known permanent cure for eczema (atopic dermatitis). It’s a chronic condition for many people, which means it tends to come and go over time. The good news is that it can be effectively managed so that you can live comfortably with minimal symptoms. Many children who have eczema early in life find that it improves or even clears up as they get older – this is sometimes referred to as “outgrowing” eczema (for example, some babies have eczema that later goes away by their teen years).
In other cases, eczema can persist into adulthood or even start in adulthood. While we can’t cure it forever, the goal of treatment is to reach long periods where the skin is clear or only mildly affected (this is called remission), and to quickly treat any flare-ups that do occur.
With the right combination of daily skincare (moisturizing and gentle care), trigger avoidance, and medicinal treatments when needed, many people keep their eczema well-controlled. There are also new therapies being developed (like special biologic medications for severe eczema) that are offering hope for even better control. So, think of eczema like a condition you have to manage – similar to asthma or allergies – sometimes you’ll forget it’s even there, other times you’ll need to give it extra attention. By staying vigilant with your skincare routine and working with a healthcare professional for a treatment plan, you can greatly reduce the impact eczema has on your life.
Conclusion:
Managing eczema-prone skin in a city like Lahore might seem daunting, but these five tips – moisturizing regularly, avoiding triggers, gentle cleansing, wearing comfy clothing, and seeking professional help when needed – can make a world of difference. The key is consistency and listening to your skin’s needs. Over time, you’ll figure out what works best for you. Remember, you don’t have to do it alone. If you’re struggling or need personalized guidance, consider reaching out to a specialist.
Take the Next Step: For those in Lahore, if your eczema is still troublesome despite your best efforts, Dr. M. Khawar Nazir at Boston Aesthetics is here to help. As a leading Lahore dermatologist with international training, Dr. Khawar Nazir can provide a thorough evaluation of your skin and craft a tailored treatment plan to get your eczema under control. Why endure itching and discomfort when an expert can offer solutions and relief? Don’t wait – healthy, calm skin is possible with the right care.
👉 Ready for healthier skin? Book an appointment with Dr. M. Khawar Nazir at Boston Aesthetics, Lahore, and take the first step toward an eczema management plan that’s perfectly designed for you. Your skin will thank you, and you’ll regain the comfort and confidence you deserve!
- Acne and Scar Treatments
- Anti-Aging Treatments by Dr. Khawar Nazir, Lahore
- Best Dermatologist in Lahore
- Best Hydrafacial in Gulberg Lahore
- Contact Us At Boston Aesthetics Lahore
- Dermatologist in Lahore – Boston Aesthetics Gulberg II
- Expert Dermatology Services in Lahore | Boston Aesthetics
- Finding the Best Skin Specialist in Lahore
- Gallery
- Glow Facial in Lahore – Radiant Skin Awaits You!
- Hair Transplant Surgery in Lahore
- Latest Skincare Trends by Dr. M. Khawar Nazir
- Medical & Advertising Disclaimer | Boston Aesthetics Lahore
- Men’s Grooming at Boston Aesthetics Lahore
- Privacy Policy
- Services by Dr. M. Khawar Nazir in Lahore
- Skin Specialist in Lahore
- Trusted Dermatologist & Skin Care Specialist in Lahore
- Your Questions Answered: FAQ
- Experienced Dermatologist in Lahore
Contact Information
Boston Aesthetics Lahore
15-A, Hali Road, Gulberg II, Lahore
For Aesthetic Treatments Appointment: 03334046479
Dr. M. Khawar Nazir, MBBS, MSc Dermatology, Boston University, USA
American Trained Dermatologist
Dermatologist, Cosmetic, LASER & Hair Transplant Surgeon
Also Available at Bahria Town Hospital
For consultations at Bahria International Hospital, Bahria Town Lahore, call at 042-111-296-297 for an appointment today.
If you can’t make it to the clinic, don’t worry—your skin health is still our priority. Dr. M. Khawar Nazir offers convenient online video consultations, allowing you to receive expert advice and personalised care from the comfort of your home. Whether you’re managing ongoing treatment or seeking advice on new concerns, our virtual consultations provide you with the same level of attention and care as an in-person visit. To book your online consultation, simply call or WhatsApp us at 03334046479.
Author Information:
Dr. M. Khawar Nazir, MBBS, MSc Dermatology, Boston University, USA
American Trained Dermatologist in Lahore
Dermatologist, Cosmetic, LASER & Hair Transplant Surgeon
Boston Aesthetics, 15-A, Hali Road, Gulberg II, Lahore | 03334046479
Your message has been sent
Disclaimer
This content is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The information provided in this blog post is based on general dermatological guidelines and expert insights from Dr. M. Khawar Nazir, an American-trained dermatologist at Boston Aesthetics, Lahore.
Individual results may vary, and eczema management should be tailored to each person’s unique skin condition. For personalized treatment and medical recommendations, please consult a qualified dermatologist or healthcare professional.
This article complies with Google Ads policies by avoiding references to prescription medications, experimental treatments, or misleading medical claims. Always seek professional advice before making any skincare or health-related decisions.
📍 For expert eczema care, book an appointment with Dr. M. Khawar Nazir at Boston Aesthetics, Lahore.







Leave a Reply